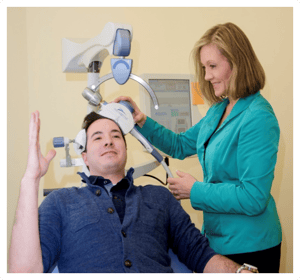
Transcranial Magnetic Stimulation (TMS) is a revolutionary treatment, approved by the FDA, for patients suffering from depression and obsessive-compulsive disorder (OCD) who have not responded to standard medications and therapy. A device placed on the patient’s head delivers targeted magnetic pulses that penetrate the scalp and skull to induce activity in brain cells (called neurons) underneath the scalp to target specific areas of the brain. TMS therapy is a non-invasive treatment, and it does not require anesthesia or sedation. Patients remain fully awake and alert during their TMS treatment sessions and they can travel independently to the clinic and continue with their day-to-day activities without limitation.
Published reports from TMS treatment studies show more than half of patients treated with TMS therapy experienced significant improvements in their symptoms and about one-third of patients experience remission. TMS treated patients have experienced significant improvements in their anxiety, functioning, pleasure, appetite changes, aches and pains, and lack of energy, and other debilitating symptoms associated with their illness.
TMS Clinic
Butler Hospital
345 Blackstone Boulevard
Delmonico 1A
Providence, RI 02906
P: (401) 455-6632
F: (401) 455-6686
Email: BRAIN@CareNE.org
Click here to begin the screening process with our TMS team.
Clinic Hours: Monday-Friday 8:00 am-5:30 pm
For Physicians
For clinicians, if you would like to refer your patient for consideration of TMS Therapy, please download and complete this form and fax to (401) 455-6686.
In October of 2008, the FDA approved the first TMS device to treat depression, and Butler Hospital’s TMS Clinic team includes researchers who have continued to study TMS since that point in time. The Butler TMS Clinic was opened to the public for non-research standard care in January 2009 and has remained one of the busiest TMS programs in the Northeast since then. Our state-of-the-art treatment facility houses multiple FDA-cleared devices for standard TMS clinical care, as well as investigational devices for research clinical trials. TMS researchers at Butler continue to conduct investigations aimed to make the TMS therapy outcomes even better and more personalized for each patient.
A typical course of TMS therapy includes:
We strive to make the process of referring patients to the Butler TMS Clinic as easy and effective as possible. Most of our patients receive TMS therapy as a covered service through their health insurance policy. As such, we go the extra mile to obtain source documentation of past treatment history.
For additional information, please click here to hear Dr. Linda Carpenter, lead TMS expert and the director of the TMS Clinic at Butler Hospital, speak about TMS Therapy.TMS
As of January 2024, the FDA has approved the use of TMS for Major Depressive Disorder (MDD), Obsessive Compulsive Disorder (OCD), and Smoking Cessation. Insurance coverage is available for MDD and OCD so please contact the clinic and our team will verify your insurance and coordinate benefits. There is extensive literature using TMS to treat other indications such as Alzheimer’s Disease, Dementia, Addictions, Executive Functioning deficits (ADD, ADHD), PTSD, Autism, Pain syndromes, and Bipolar Disorder are backed by scientific evidence and has shown TMS can be used off-label to alleviate and/or treat illnesses. This may be available on a self-pay basis and can be discussed on a case-by-case basis.
TMS treatment for depression is covered by nearly all insurance carriers including Medicare and Medicaid. A screening process is used to determine whether each patient meets their insurance policy’s coverage criteria. An outpatient appointment, called a TMS Consultation visit, takes place with a TMS provider prior to starting the course of TMS therapy. When a patient is determined to be eligible, our TMS Clinic staff will submit the required pre-authorization information and work with insurance companies to obtain coverage.
Typical eligibility requirements for insurance coverage of TMS include a patient:
To find out if you are candidate for TMS, you can begin the screening process by calling (401) 455-6632 or by filling out the form below and someone on the team will be in contact with you shortly.
TMS is non-invasive and does not involve surgery or insertion of intravenous lines or anything else put into your body.
Over 10,000 active TMS treatments were safely performed during clinical trials with the type of TMS device used at Butler Hospital.
Counting calories is a great strategy when trying to lose or maintain your weight, but the question is how high should you be counting?
Before TMS:
After TMS:
Before TMS:
After TMS:
Before TMS:
After TMS:
Since 2015, the TMS Clinical Service has been closely integrated with the Neuromodulation Research division at Butler Hospital with its goal to bridge the gap between scientific research and clinical practice in non-invasive brain stimulation. The incorporation of research findings with clinical expertise is crucial to help inform TMS practitioners into providing the best care and to enhance patient outcomes. This research has expanded beyond TMS to include other forms of brain stimulation such as using wearable devices and to gain a better understanding into other clinical services we offer such as Esketamine and ECT. These procedures may include the collection of brain imaging (MRI, EEG), blood biomarkers, physiological data (heart rate, nerve conduction, blood pressure), working memory, behavioral, and cognitive tasks, ecological momentary assessments, and the use of other psychometric surveys to help us investigate potential biomarkers into clinical response and develop ways to personalize treatment.
The Neuromodulation Research program at Butler shares a close connection with Butler Hospital COBRE (Center of Biomedical Research Excellence) for Neuromodulation with shared research goals to support innovative clinical research in neuromodulation (i.e., brain stimulation) and career development of investigators in the field.
TMS is non-invasive, does not involve the insertion of intravenous lines or surgery, and does not require any anesthesia or sedation.
Over 10,000 TMS treatments were safely performed during clinical trials with the type of TMS device used at Butler Hospital.
Have questions about what to expect as a patient or who will be involved in the treatment? We've got you covered.
Director, Butler TMS Clinic and Neuromodulation Research Facility
Linda L. Carpenter, MD is a Professor of Psychiatry in the Alpert Medical School of Brown University and Chief of the Mood Disorders Program at Butler Hospital. She completed her undergraduate degree at the University of Michigan and medical school at the University of Pennsylvania. She did an internship in internal medicine, psychiatry residency, and research fellowship at Yale, and then joined the faculty of the Department of Psychiatry and Human Behavior, Alpert Medical School of Brown University in 1997.
She has continued her path since then as a physician-researcher investigating the neurobiology of, and new treatments for, major depression and other mood and anxiety disorders. Dr. Carpenter has also conducted a number of randomized clinical trials sponsored by industry and NIH, investigating investigational drugs and devices for treating depression, including esketamine, Vagus Nerve Stimulation (VNS), Deep Brain Stimulation (DBS), Transcranial Magnetic Stimulation (TMS) and transcranial Direct Current Stimulation (tDCS). She is the founding Director of the Butler Hospital TMS Clinic and Neuromodulation Research Facility and co-author of several published TMS Clinical practice guidelines. Dr. Carpenter was engaged in TMS research prior to the first FDA clearance in 2008, and has remained active as a TMS clinician and researcher since then. She is a faculty member of several national TMS training courses and has served in various leadership roles for the Clinical TMS Society. She is a member of the American Psychiatric Association (APA) Council on Research, past President of the Society of Biological Psychiatry (SOBP), and has published extensively on TMS and other treatments for depression.
Clinical and Research Nurse
Ms. Melissa Burt graduated with a Bachelor of Science in Human Development and Family Studies from the University of Rhode Island (URI) in 1996. She completed an internship while at URI at Butler Hospital’s partial hospital in 1996 then shortly after, she was hired as a mental health worker. She then received her CNA license and subsequently her RN license in 2004.
Dr. Benjamin Greenberg has a BA in psychology from Amherst College, a PhD in neurosciences from UC San Diego, and an MD from the University of Miami, with psychiatry residency at Johns Hopkins. He then led adult OCD research at NIMH, where he performed the first transcranial magnetic stimulation (TMS) study in that illness. At Butler Hospital and Brown since 2000, he has focused on invasive neurosurgeries including ventral capsulotomy and deep brain stimulation (DBS).
FDA humanitarian approval of DBS for intractable OCD in 2009 was based on that work. His NIH funding has included R21, R01, U01, P50, and P20 grants. He has a secondary focus in psychiatric genetics. As a clinical psychiatrist, he has treated OCD for thirty years; and over the past five years has also treated PTSD, he previously led Butler outpatient services. He currently directs the COBRE Center for Neuromodulation at Butler Hospital and co-directs the Center for Neuromodulation and Neurotechnology (CfNN) at the Providence VAMC (PVAMC), in both roles focusing on noninvasive brain stimulation.
Dr. Amy Halt received her MD and PhD in Pharmacology from the University of Iowa. She then moved to Brown University, where she completed adult psychiatry residency training as well as a geriatric psychiatry fellowship. She is a Clinical Assistant Professor in the Dept. of Psychiatry and Human Behavior at Brown University. She has been an attending inpatient psychiatrist at Butler Hospital since 2014.
Currently, she is the Unit Chief of the Senior Specialty Unit. She is active in teaching at all levels of medical training, including supervising medical students, adult psychiatry residents, and geriatric fellows (psychiatry and medicine) on the geriatric inpatient unit. She is also the Education Coordinator for the Brown Geriatric Psychiatry Fellowship.
Dr. Lawrence Price attended the University of Michigan, where he received a B.S. with highest honors in psychology and high distinction in 1974, followed by an M.D. in 1978. After an internship in internal medicine at Norwalk Hospital, he completed a residency and fellowship in psychiatry at Yale University. From 1982 until 1996, Dr. Price was on the faculty in the Department of Psychiatry at Yale University, where he served as Associate Professor and Director of the Clinical Neuroscience Research Unit at the Connecticut Mental Health Center.
Since 1996, he has been Professor of Psychiatry at Brown University. From 1996 to 2012, he was Clinical Director, Director of Research, and Chair of the Institutional Review Board at Butler Hospital in Providence, Rhode Island, subsequently serving as Chief Medical Officer from 2012 until 2014. He was President of Butler Hospital and Executive Chief of the Brain and Behavioral Health Service Line of Care New England from 2014 until 2017. He was identified by the Institute for Scientific Information as one of the top ten authors of high-impact papers in psychiatry from 1990 to 1999. In addition to his research activities, Dr. Price has received numerous awards for his teaching and clinical work, and is Editor of the Brown University Psychopharmacology Update and Editor (with I. Stolerman) of the Encyclopedia of Psychopharmacology, Second Edition.
Dr. Brian Tesar received a B.A. with honors in Chemistry from the University of Chicago in 1987. He studied medicine and biochemistry and received his M.D. from the University of Illinois in 1992. Dr. Tesar completed a psychiatric residency program with Washington University in St. Louis in 1996.
After completing his training, Dr. Tesar cared for patients in a variety of roles: as staff psychiatrist and day hospital medical director at the Cape Cod and Islands Community Mental Health Center(1996-2000), as medical director of Gosnold on Cape Cod outpatient clinics(2000-2004), as staff psychiatrist for AHRC New York(2005-2009), and as medical director of the Kent Hospital (Warwick, RI) psychiatric care unit (2009-2017). Since 2017, Dr. Tesar has served as staff psychiatrist at Butler Hospital (Providence, RI) in both the inpatient and partial hospital programs. Dr. Tesar is also a self-taught computer programmer whose experience includes development of a database system and dynamically driven website for a real estate company in New York City. Dr. Tesar has a strong interest in developing computer systems that enhance psychiatric care.
TMS Clinical Supervisor/Neuromodulation Research Facility Coordinator
Mr. Eric Tirrell completed his undergraduate degree in psychology at the University of Rhode Island. He is the TMS and Esketamine clinical supervisor of Butler Hospital’s TMS Clinic and has been providing TMS treatment for neuropsychiatric disorders for over 8 years. He has extensive experience with all aspects of TMS clinical care and he is well versed in operating Neurostar, Magstim, Nexstim, MagnMore, Magventure and other investigational TMS device systems using a variety of TMS protocols and coils.
In addition to his role on the TMS and Esketamine clinical service, Eric also serves as the Research Coordinator for Butler’s Neuromodulation Research Facility and has led a wide range of studies in individuals across the lifespan. He works with Butler Hospital and Brown University-based faculty within the Department of Psychiatry and Human Behavior and their research staff in Butler’s COBRE Center for Neuromodulation to incorporate noninvasive brain stimulation and imaging techniques into their clinical research. He has had extensive training in the collection of physiological data and brain imaging for biomarker development and investigating brain network function and connectivity. His goals are to help develop optimized individual neuromodulation approaches for depression and to ultimately use TMS as a treatment modality for a wide range of conditions and disorders.
Dr. Audrey Tyrka received her MD and PhD in medicine and psychology through a combined program at the University of Pennsylvania. She completed the psychiatry residency at the Warren Alpert Medical School of Brown University with research training in clinical neuroscience. She is the Director of Research at Butler hospital, and also directs our Laboratory for Clinical and Translational Neuroscience.
Dr. Tyrka is Professor of Psychiatry and Human Behavior at Brown and Director of the NIMH-funded R25 Research Training Program in the Brown psychiatry residency program. Co-Director of the Initiative on Stress, Trauma, and Resilience in the Brown Department of Psychiatry and Human Behavior, Dr. Tyrka's program of research is focused on discovering the social, behavioral and molecular mechanisms of risk and resilience in children and adults with a history of early adversity and trauma. She also has interest and experience with research and clinical work using neuromodulation approaches to treat depression and post-traumatic stress disorder, and is an attending psychiatrist in our TMS program.
Copyright © 2023 Care New England Health System